Research Behind Face Transplant
Ethics and Consent
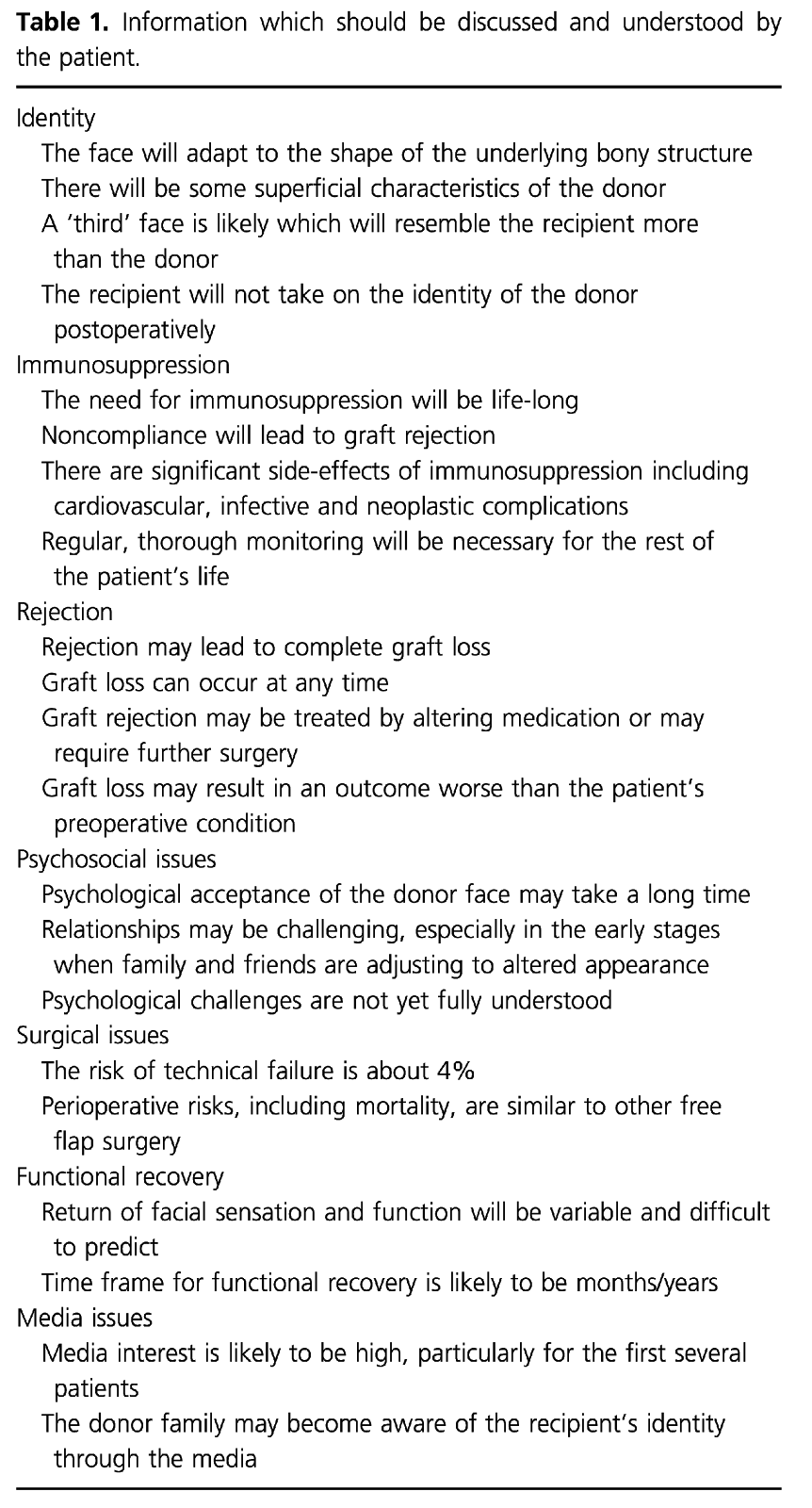
With any procedure, all the risks, benefits, and alternatives are discussed thoroughly between the treating physician and patient. This is called the informed consent process. With regards to face transplantation, however, the informed consent process is less well defined as it is an experimental procedure. There are still many unknowns with regards to the benefits, long term outcomes, immediate and long term risks from the procedure and life-long immunosuppression. Therefore, much discussion has taken place as to whether or not facial transplantation is even ethical.
If facial transplantation is already a consideration for the patient, then their deficit must be of such severity that conventional reconstructive methods have already failed or would be a wholly inadequate or unacceptable result, both functionally and aesthetically.
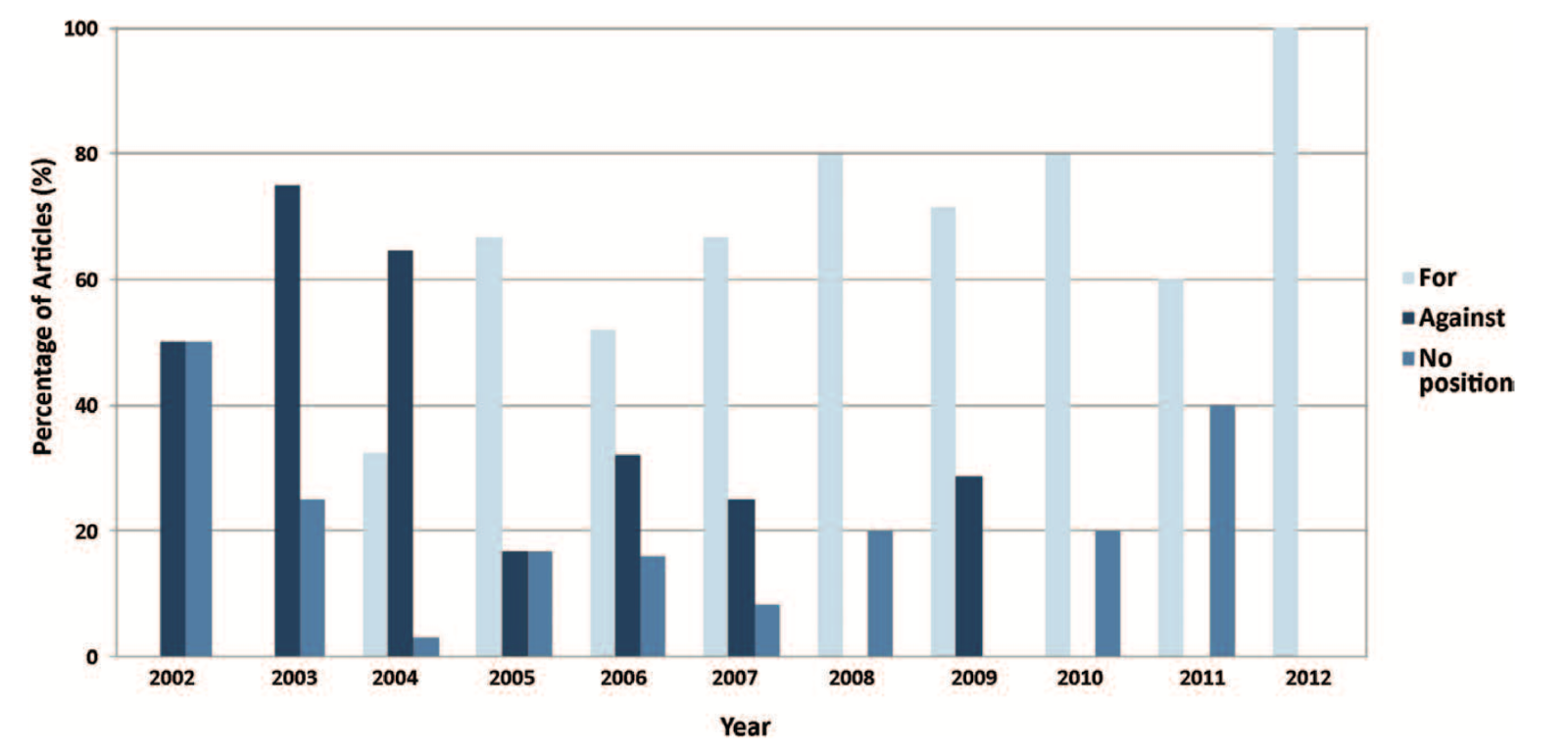
Prior to the first face transplant in 2005, the procedure was condemned from an ethical standpoint and that the risks outweighed the benefits. After the first transplant was completed and more discussion took place and as more and more favorable outcomes come about from subsequent surgeries, there was a shift in attitude. Nowadays, many institutions are pushing forward with face transplant protocols of their own to help patients who were deemed unsalvageable only a decade ago.
Kiwanuka, H. et al. Evolution of ethical debate on face transplantation. Plast Reconstr Surg 132, 1558-1568 (2013).
Renshaw, A., Clarke, A., Diver, A. J., Ashcroft, R. E. & Butler, P. E. Informed consent for facial transplantation. Transpl Int 19, 861-867 (2006).
Basic Science
Facial transplantation was first performed on rats and mice and much was learned about the technical feasibility of the procedure. Also, much was learned about the reinnervation potential for sensory and motor potential. Studies in rats and mice have shown that transplanted faces are able to achieve motor control and also feel touch.
In addition, numerous immunologic studies were carried out to determine the immunologic consequence of the procedure since skin, bone, and other tissues are transplanted. Ideally, the recipient’s immune system can be modified to tolerate the transplanted graft but currently, that is not possible. As such, life-long immunosuppression strategies are most commonly used post-transplant.
Many cadaveric dissections were also performed to determine the best surgical approach for harvest and which vessels were required to provide adequate perfusion of the graft.